| Myocardial infarction | |
|---|---|
| Classification and external resources | |
 Diagram of a myocardial infarction (2) of the tip of the anterior wall of the heart (an apical infarct) after occlusion (1) of a branch of the left coronary artery (LCA, right coronary artery = RCA). | |
| ICD-10 | I21.-I22. |
| ICD-9 | 410 |
| DiseasesDB | 8664 |
| MedlinePlus | 000195 |
| eMedicine | med/1567 emerg/327 ped/2520 |
| MeSH | D009203 |
Classical symptoms of acute myocardial infarction include sudden chest pain (typically radiating to the left arm or left side of the neck), shortness of breath, nausea, vomiting, palpitations, sweating, and anxiety (often described as a sense of impending doom).[1] Women may experience fewer typical symptoms than men, most commonly shortness of breath, weakness, a feeling of indigestion, and fatigue.[2] Approximately one quarter of all myocardial infarctions are "silent", without chest pain or other symptoms.
Among the diagnostic tests available to detect heart muscle damage are an electrocardiogram (ECG), echocardiography, and various blood tests. The most often used markers are the creatine kinase-MB (CK-MB) fraction and the troponin levels. Immediate treatment for suspected acute myocardial infarction includes oxygen, aspirin, and sublingual nitroglycerin.[3]
Most cases of STEMI (ST elevation MI) are treated with thrombolysis or percutaneous coronary intervention (PCI). NSTEMI (non-ST elevation MI) should be managed with medication, although PCI is often performed during hospital admission. In people who have multiple blockages and who are relatively stable, or in a few emergency cases, bypass surgery may be an option.
Heart attacks are the leading cause of death for both men and women worldwide.[4] Important risk factors are previous cardiovascular disease, older age, tobacco smoking, high blood levels of certain lipids (triglycerides, low-density lipoprotein) and low levels of high density lipoprotein (HDL), diabetes, high blood pressure, obesity, chronic kidney disease, heart failure, excessive alcohol consumption, the abuse of certain drugs (such as cocaine and methamphetamine), and chronic high stress levels.[5][6]
Contents
|
Classification
There are two basic types of acute myocardial infarction:- Transmural: associated with atherosclerosis involving major coronary artery. It can be subclassified into anterior, posterior, or inferior. Transmural infarcts extend through the whole thickness of the heart muscle and are usually a result of complete occlusion of the area's blood supply.[7]
- Subendocardial: involving a small area in the subendocardial wall of the left ventricle, ventricular septum, or papillary muscles. Subendocardial infarcts are thought to be a result of locally decreased blood supply, possibly from a narrowing of the coronary arteries. The subendocardial area is farthest from the heart's blood supply and is more susceptible to this type of pathology.[7]
The phrase "heart attack" is sometimes used incorrectly to describe sudden cardiac death, which may or may not be the result of acute myocardial infarction. A heart attack is different from, but can be the cause of cardiac arrest, which is the stopping of the heartbeat, and cardiac arrhythmia, an abnormal heartbeat. It is also distinct from heart failure, in which the pumping action of the heart is impaired; severe myocardial infarction may lead to heart failure, but not necessarily.[citation needed]
A 2007 consensus document classifies myocardial infarction into five main types:[9]
- Type 1 – Spontaneous myocardial infarction related to ischaemia due to a primary coronary event such as plaque erosion and/or rupture, fissuring, or dissection
- Type 2 – Myocardial infarction secondary to ischaemia due to either increased oxygen demand or decreased supply, e.g. coronary artery spasm, coronary embolism, anaemia, arrhythmias, hypertension, or hypotension
- Type 3 – Sudden unexpected cardiac death, including cardiac arrest, often with symptoms suggestive of myocardial ischaemia, accompanied by presumably new ST elevation, or new LBBB, or evidence of fresh thrombus in a coronary artery by angiography and/or at autopsy, but death occurring before blood samples could be obtained, or at a time before the appearance of cardiac biomarkers in the blood
- Type 4 – Associated with coronary angioplasty or stents:
- Type 4a – Myocardial infarction associated with PCI
- Type 4b – Myocardial infarction associated with stent thrombosis as documented by angiography or at autopsy
- Type 5 – Myocardial infarction associated with CABG
Signs and symptoms
Shortness of breath (dyspnea) occurs when the damage to the heart limits the output of the left ventricle, causing left ventricular failure and consequent pulmonary edema. Other symptoms include diaphoresis (an excessive form of sweating),[1] weakness, light-headedness, nausea, vomiting, and palpitations. These symptoms are likely induced by a massive surge of catecholamines from the sympathetic nervous system[12] which occurs in response to pain and the hemodynamic abnormalities that result from cardiac dysfunction. Loss of consciousness (due to inadequate cerebral perfusion and cardiogenic shock) and sudden death (frequently due to the development of ventricular fibrillation) can occur in myocardial infarctions.[citation needed]
Women and older patients report atypical symptoms more frequently than their male and younger counterparts.[13] Women also report more numerous symptoms compared with men (2.6 on average vs 1.8 symptoms in men).[13] The most common symptoms of MI in women include dyspnea (shortness of breath), weakness, and fatigue. Fatigue, sleep disturbances, and dyspnea have been reported as frequently occurring symptoms which may manifest as long as one month before the actual clinically manifested ischemic event. In women, chest pain may be less predictive of coronary ischemia than in men.[14]
Approximately one fourth of all myocardial infarctions are silent, without chest pain or other symptoms.[15] These cases can be discovered later on electrocardiograms, using blood enzyme tests or at autopsy without a prior history of related complaints. A silent course is more common in the elderly, in patients with diabetes mellitus[16] and after heart transplantation, probably because the donor heart is not fully innervated by the nervous system of the recipient.[17] In diabetics, differences in pain threshold, autonomic neuropathy, and psychological factors have been cited as possible explanations for the lack of symptoms.[16]
Any group of symptoms compatible with a sudden interruption of the blood flow to the heart are called an acute coronary syndrome.[18]
The differential diagnosis includes other catastrophic causes of chest pain, such as pulmonary embolism, aortic dissection, pericardial effusion causing cardiac tamponade, tension pneumothorax, and esophageal rupture. Other non-catastrophic differentials include gastroesophageal reflux and Tietze's syndrome.[19]
Causes
Heart attack rates are higher in association with intense exertion, be it psychological stress or physical exertion, especially if the exertion is more intense than the individual usually performs.[20] Quantitatively, the period of intense exercise and subsequent recovery is associated with about a 6-fold higher myocardial infarction rate (compared with other more relaxed time frames) for people who are physically very fit.[20] For those in poor physical condition, the rate differential is over 35-fold higher.[20] One observed mechanism for this phenomenon is the increased arterial pulse pressure stretching and relaxation of arteries with each heart beat which, as has been observed with intravascular ultrasound, increases mechanical "shear stress" on atheromas and the likelihood of plaque rupture.[20]Acute severe infection, such as pneumonia, can trigger myocardial infarction. A more controversial link is that between Chlamydophila pneumoniae infection and atherosclerosis.[21] While this intracellular organism has been demonstrated in atherosclerotic plaques, evidence is inconclusive as to whether it can be considered a causative factor.[21] Treatment with antibiotics in patients with proven atherosclerosis has not demonstrated a decreased risk of heart attacks or other coronary vascular diseases.[22]
There is an association of an increased incidence of a heart attack in the morning hours, more specifically around 9 a.m.[23][24][25] Some investigators have noticed that the ability of platelets to aggregate varies according to a circadian rhythm, although they have not proven causation.[26]
Risk factors
Risk factors for atherosclerosis are generally risk factors for myocardial infarction:[citation needed]- Diabetes (with or without insulin resistance) – the single most important risk factor for ischaemic heart disease (IHD)
- Tobacco smoking
- Hypercholesterolemia (more accurately hyperlipoproteinemia, especially high low density lipoprotein and low high density lipoprotein)
- Low HDL
- High Triglycerides
- High blood pressure
- Family history of ischaemic heart disease (IHD)
- Obesity[27] (defined by a body mass index of more than 30 kg/m², or alternatively by waist circumference or waist-hip ratio).
- Age: Men acquire an independent risk factor at age 45, Women acquire an independent risk factor at age 55; in addition individuals acquire another independent risk factor if they have a first-degree male relative (brother, father) who suffered a coronary vascular event at or before age 55. Another independent risk factor is acquired if one has a first-degree female relative (mother, sister) who suffered a coronary vascular event at age 65 or younger.
- Hyperhomocysteinemia (high homocysteine, a toxic blood amino acid that is elevated when intakes of vitamins B2, B6, B12 and folic acid are insufficient)
- Stress (occupations with high stress index are known to have susceptibility for atherosclerosis)
- Alcohol Studies show that prolonged exposure to high quantities of alcohol can increase the risk of heart attack
- Males are more at risk than females.[20]
Socioeconomic factors such as a shorter education and lower income (particularly in women), and unmarried cohabitation may also contribute to the risk of MI.[29] To understand epidemiological study results, it's important to note that many factors associated with MI mediate their risk via other factors. For example, the effect of education is partially based on its effect on income and marital status.[29]
Women who use combined oral contraceptive pills have a modestly increased risk of myocardial infarction, especially in the presence of other risk factors, such as smoking.[30]
Inflammation is known to be an important step in the process of atherosclerotic plaque formation.[31] C-reactive protein (CRP) is a sensitive but non-specific marker for inflammation. Elevated CRP blood levels, especially measured with high sensitivity assays, can predict the risk of MI, as well as stroke and development of diabetes.[31] Moreover, some drugs for MI might also reduce CRP levels.[31] The use of high sensitivity CRP assays as a means of screening the general population is advised against, but it may be used optionally at the physician's discretion, in patients who already present with other risk factors or known coronary artery disease.[32] Whether CRP plays a direct role in atherosclerosis remains uncertain.[31]
Inflammation in periodontal disease may be linked to coronary heart disease, and since periodontitis is very common, this could have great consequences for public health.[33] Serological studies measuring antibody levels against typical periodontitis-causing bacteria found that such antibodies were more present in subjects with coronary heart disease.[34] Periodontitis tends to increase blood levels of CRP, fibrinogen and cytokines;[35] thus, periodontitis may mediate its effect on MI risk via other risk factors.[36] Preclinical research suggests that periodontal bacteria can promote aggregation of platelets and promote the formation of foam cells.[37][38] A role for specific periodontal bacteria has been suggested but remains to be established.[39] There is some evidence that influenza may trigger a acute myocardial infarction.[40]
Baldness, hair greying, a diagonal earlobe crease (Frank's sign[41]) and possibly other skin features have been suggested as independent risk factors for MI.[42] Their role remains controversial; a common denominator of these signs and the risk of MI is supposed, possibly genetic.[43]
Calcium deposition is another part of atherosclerotic plaque formation. Calcium deposits in the coronary arteries can be detected with CT scans. Several studies have shown that coronary calcium can provide predictive information beyond that of classical risk factors.[44][45][46]
The European Society of Cardiology and the European Association for Cardiovascular Prevention and Rehabilitation have developed an interactive tool for prediction and managing the risk of heart attack and stroke in Europe. HeartScore is aimed at supporting clinicians in optimising individual cardiovascular risk reduction. The Heartscore Programme is available in 12 languages and offers web based or PC version.[47]
Pathophysiology
See also: Acute coronary syndrome
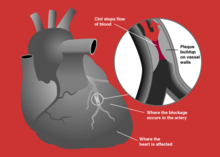
A myocardial infarction occurs when an atherosclerotic plaque slowly builds up in the inner lining of a coronary artery and then suddenly ruptures, causing catastrophic thrombus formation, totally occluding the artery and preventing blood flow downstream.
If impaired blood flow to the heart lasts long enough, it triggers a process called the ischemic cascade; the heart cells in the territory of the occluded coronary artery die (chiefly through necrosis) and do not grow back. A collagen scar forms in its place. Recent studies indicate that another form of cell death called apoptosis also plays a role in the process of tissue damage subsequent to myocardial infarction.[52] As a result, the patient's heart will be permanently damaged. This Myocardial scarring also puts the patient at risk for potentially life threatening arrhythmias, and may result in the formation of a ventricular aneurysm that can rupture with catastrophic consequences.
Injured heart tissue conducts electrical impulses more slowly than normal heart tissue. The difference in conduction velocity between injured and uninjured tissue can trigger re-entry or a feedback loop that is believed to be the cause of many lethal arrhythmias. The most serious of these arrhythmias is ventricular fibrillation (V-Fib/VF), an extremely fast and chaotic heart rhythm that is the leading cause of sudden cardiac death. Another life threatening arrhythmia is ventricular tachycardia (V-Tach/VT), which may or may not cause sudden cardiac death. However, ventricular tachycardia usually results in rapid heart rates that prevent the heart from pumping blood effectively. Cardiac output and blood pressure may fall to dangerous levels, which can lead to further coronary ischemia and extension of the infarct.
The cardiac defibrillator is a device that was specifically designed to terminate these potentially fatal arrhythmias. The device works by delivering an electrical shock to the patient in order to depolarize a critical mass of the heart muscle, in effect "rebooting" the heart. This therapy is time dependent, and the odds of successful defibrillation decline rapidly after the onset of cardiopulmonary arrest.
Diagnosis
Main article: Myocardial infarction diagnosis
The diagnosis of myocardial infarction can be made after assessing patient's complaints and physical status. ECG changes, coronary angiogram and levels of cardiac markers help to confirm the diagnosis. ECG gives valuable clues to identify the site of myocardial damage while coronary angiogram allows visualization of narrowing or obstructions in the heart vessels.[53] At autopsy, a pathologist can diagnose a myocardial infarction based on anatomopathological findings.A chest radiograph and routine blood tests may indicate complications or precipitating causes and are often performed upon arrival to an emergency department. New regional wall motion abnormalities on an echocardiogram are also suggestive of a myocardial infarction. Echo may be performed in equivocal cases by the on-call cardiologist.[54] In stable patients whose symptoms have resolved by the time of evaluation, Technetium (99mTc) sestamibi (i.e. a "MIBI scan") or thallium-201 chloride can be used in nuclear medicine to visualize areas of reduced blood flow in conjunction with physiologic or pharmocologic stress.[54][55] Thallium may also be used to determine viability of tissue, distinguishing whether non-functional myocardium is actually dead or merely in a state of hibernation or of being stunned.[56]
WHO criteria[57] formulated in 1979 have classically been used to diagnose MI; a patient is diagnosed with myocardial infarction if two (probable) or three (definite) of the following criteria are satisfied:
- Clinical history of ischaemic type chest pain lasting for more than 20 minutes
- Changes in serial ECG tracings
- Rise and fall of serum cardiac biomarkers such as creatine kinase-MB fraction and troponin
Prevention
The risk of a recurrent myocardial infarction decreases with strict blood pressure management and lifestyle changes, chiefly smoking cessation, regular exercise, a sensible diet for patients with heart disease, and limitation of alcohol intake.Patients are usually commenced on several long-term medications post-MI, with the aim of preventing secondary cardiovascular events such as further myocardial infarctions, congestive heart failure or cerebrovascular accident (CVA). Unless contraindicated, such medications may include:[59][60]
- Evidence supports the consumption of polyunsaturated fats instead of saturated fats as a measure of decreasing coronary heart disease.[61]
- Antiplatelet drug therapy such as aspirin and/or clopidogrel should be continued to reduce the risk of plaque rupture and recurrent myocardial infarction. Aspirin is first-line, owing to its low cost and comparable efficacy, with clopidogrel reserved for patients intolerant of aspirin. The combination of clopidogrel and aspirin may further reduce risk of cardiovascular events, however the risk of hemorrhage is increased.[62]
- Beta blocker therapy such as metoprolol or carvedilol should be commenced.[63] These have been particularly beneficial in high-risk patients such as those with left ventricular dysfunction and/or continuing cardiac ischaemia.[64] β-Blockers decrease mortality and morbidity. They also improve symptoms of cardiac ischemia in NSTEMI.
- ACE inhibitor therapy should be commenced 24–48 hours post-MI in hemodynamically-stable patients, particularly in patients with a history of MI, diabetes mellitus, hypertension, anterior location of infarct (as assessed by ECG), and/or evidence of left ventricular dysfunction. ACE inhibitors reduce mortality, the development of heart failure, and decrease ventricular remodelling post-MI.[65]
- Statin therapy has been shown to reduce mortality and morbidity post-MI.[66][67] The effects of statins may be more than their LDL lowering effects. The general consensus is that statins have plaque stabilization and multiple other ("pleiotropic") effects that may prevent myocardial infarction in addition to their effects on blood lipids.[68]
- The aldosterone antagonist agent eplerenone has been shown to further reduce risk of cardiovascular death post-MI in patients with heart failure and left ventricular dysfunction, when used in conjunction with standard therapies above.[69] Spironolactone is another option that is sometimes preferable to eplerenone due to cost.
- Omega-3 fatty acids, commonly found in fish, have been shown to reduce mortality post-MI.[70] While the mechanism by which these fatty acids decrease mortality is unknown, it has been postulated that the survival benefit is due to electrical stabilization and the prevention of ventricular fibrillation.[71] However, further studies in a high-risk subset have not shown a clear-cut decrease in potentially fatal arrhythmias due to omega-3 fatty acids.[72][73]
A Cochrane review found that giving heparin to people who have heart conditions like unstable angina and some forms of heart attack reduces the risk of having another heart attack. However, heparin also increases the chance of suffering from minor bleeding.[75]
Management
Main article: Myocardial infarction management
An MI is a medical emergency which requires immediate medical attention. Treatment attempts to salvage as much myocardium as possible and to prevent further complications, thus the phrase "time is muscle".[76] Oxygen, aspirin, and nitroglycerin may be administered. Morphine was classically used if nitroglycerin was not effective; however, it may increase mortality in the setting of NSTEMI.[77] A 2009 and 2010 review of high flow oxygen in myocardial infarction found increased mortality and infarct size, calling into question the recommendation about its routine use.[78][79] Percutaneous coronary intervention (PCI) or fibrinolysis are recommended in those with an STEMI.Complications
Main article: Myocardial infarction complications
Complications may occur immediately following the heart attack (in the acute phase), or may need time to develop (a chronic problem). Acute complications may include heart failure if the damaged heart is no longer able to adequately pump blood around the body; aneurysm or rupture of the myocardium; mitral regurgitation, particularly if the infarction causes dysfunction of the papillary muscle; and arrhythmias, such as ventricular fibrillation, ventricular tachycardia, atrial fibrillation and heart block. Longer-term complications include heart failure, atrial fibrillation, and the increased risk of a second myocardial infarction.Prognosis
The prognosis post myocardial infarction varies greatly, depending on a person's health, the extent of the heart damage and the treatment given. For the period 2005 – 2008 in the United States the median mortality at 30 days was 16.6% with a range from 10.9% to 24.9% depending on the hospital.[80] Using variables available in the emergency room, people with a higher risk of adverse outcome can be identified. One study found that 0.4% of patients with a low risk profile died after 90 days, whereas in high risk people it was 21.1%.[81]Some of the more reproduced risk stratifying factors include: age, hemodynamic parameters (such as heart failure, cardiac arrest on admission, systolic blood pressure, or Killip class of two or greater), ST-segment deviation, diabetes, serum creatinine, peripheral vascular disease and elevation of cardiac markers.[81][82][83] Assessment of left ventricular ejection fraction may increase the predictive power.[84] The prognostic importance of Q-waves is debated.[85] Prognosis is significantly worsened if a mechanical complication such as papillary muscle or myocardial free wall rupture occur.[86] Morbidity and mortality from myocardial infarction has improved over the years due to better treatment.[87]
Epidemiology
Myocardial infarction is a common presentation of ischemic heart disease. The WHO estimated in 2002, that 12.6 percent of worldwide deaths were from ischemic heart disease[4] with it the leading cause of death in developed countries, and third to AIDS and lower respiratory infections in developing countries.[88] Worldwide more than 3 million people have STEMIs and 4 million have NSTEMIs a year.[89]Coronary heart disease is responsible for 1 in 5 deaths in the United States. It is becoming more common in the developing world such that in India, cardiovascular disease (CVD) is the leading cause of death.[90] The deaths due to CVD in India were 32% of all deaths in 2007 and are expected to rise from 1.17 million in 1990 and 1.59 million in 2000 to 2.03 million in 2010.[91] Although a relatively new epidemic in India, it has quickly become a major health issue with deaths due to CVD expected to double during 1985–2015.[92][93] Mortality estimates due to CVD vary widely by state, ranging from 10% in Meghalaya to 49% in Punjab (percentage of all deaths). Punjab (49%), Goa (42%), Tamil Nadu (36%) and Andhra Pradesh (31%) have the highest CVD related mortality estimates.[94] State-wise differences are correlated with prevalence of specific dietary risk factors in the states. Moderate physical exercise is associated with reduced incidence of CVD in India (those who exercise have less than half the risk of those who don't).[92]
Legal implications
At common law, a myocardial infarction is generally a disease, but may sometimes be an injury. This has implications for no-fault insurance schemes such as workers' compensation. A heart attack is generally not covered;[95] however, it may be a work-related injury if it results, for example, from unusual emotional stress or unusual exertion.[96] Additionally, in some jurisdictions, heart attacks suffered by persons in particular occupations such as police officers may be classified as line-of-duty injuries by statute or policy. In some countries or states, a person who has suffered from a myocardial infarction may be prevented from participating in activity that puts other people's lives at risk, for example driving a car or flying an airplane.[97]Research
Patients who receive stem cell treatment by coronary artery injections of stem cells derived from their own bone marrow after a myocardial infarction (MI) show improvements in left ventricular ejection fraction and end-diastolic volume not seen with placebo. The larger the initial infarct size, the greater the effect of the infusion. Clinical trials of progenitor cell infusion as a treatment approach to ST elevation MI are proceeding.[98]There are currently 3 biomaterial and tissue engineering approaches for the treatment of MI, but these are in an even earlier stage of medical research, so many questions and issues need to be addressed before they can be applied to patients. The first involves polymeric left ventricular restraints in the prevention of heart failure. The second utilizes in vitro engineered cardiac tissue, which is subsequently implanted in vivo. The final approach entails injecting cells and/or a scaffold into the myocardium to create in situ engineered cardiac tissue.[99]




No comments:
Post a Comment